From decorative tissue boxes to puppies: first lessons from my OT fieldwork internship
It’s an exciting time in my life – in the last 3 months I finished the classroom portion of my Masters in occupational therapy, got married and went on a wonderful honeymoon, and started my first occupational therapy fieldwork internship.
After I finish two full time, three-month internships*, I will officially graduate with my Masters and be qualified to sit for the board exam. This is the last step before I can actually be an OT in the real world!
My Skilled Nursing Facility (SNF) houses mostly geriatric patients who are rehabilitating from a variety of physical ailments, from hip replacements to strokes. The occupational therapist’s role in this setting is to help empower the patient to resume as much of their “prior level of function” (PLOF) as possible so they can return to their desired environment.
I feel so honored to be able to serve patients during a difficult time in their lives. I’ve learned so much already and would like to share just a few insights with you now – I can’t wait for more to come over the next 10 weeks!
1) Lesson #1: Sometimes, a decorative tissue box is not just a decorative tissue box (or, “forays into the art of observation”).
Observation is at the heart of the occupational therapy practice. We are trained to acutely observe and break down every component of an activity, and observations help us determine which aspects of the person’s physical or psychological make-up contribute to their “performance deficits” (problems doing things that are important in their lives). Our interventions target those areas that negatively affect their performance; our eyes, ears and hands (plus the cognitive tools of activity analysis) are the X-ray machines of our profession.
At some point, however, we must prioritize which elements are most important to attend to in the patient’s care. This can be a real struggle for students as initially it can appear that everything we’ve observed is important! In just 2 weeks, however, I’ve learned that even the most seemingly frivolous things can actually illuminate important aspects of a patient’s needs, condition, and motivation.
Enter the decorative tissue box. I had a patient who, early on in her stay at the SNF, was very distressed that her caregiver had forgotten to bring her decorative tissue box to her room.
At first glance (and given this patient’s physical condition), one might think a tissue box was the most superfluous detail for me to attend to. However, it ultimately ended up telling me a lot about this patient (details which I cannot publicly reveal due to privacy concerns). In the big picture, this experience showed me the following:
- Being surrounded by a sense of home and normalcy during a tumultuous time in one’s life can be very important for one’s attitude and healing;
- It’s not always about the item itself that is important but whether the person feels like their desires are valued and respected (a medical staff person will, understandably, be focused on aspects of the patient’s rehabilitation other than their room decoration; this is where caregivers and family members can provide a helping hand);
- At the end of the day, it was partly about the box itself, but more about control, which is important to remember if patients make seemingly “silly” requests.
There are so many things a patient recovery from a physical injury cannot control. The fact that this patient fought for her tissue box represented something potentially deeper about her; it told me that maybe she was not going to go down without a fight, and that she wasn’t ready to give up everything important to her just because she’d lost part of her health. If someone is willing to fight for a tissue box, it’s not too far a leap to presume that they would want to fight for their health and recovery as well.
At the most basic level, it taught me that I must not jump to quickly to cast off something seemingly superficial as unimportant. After this particular experience and upon hearing many other patients profess other very specific, aesthetic related desires, I’ve learned that it’s not my place to decide what is important and what is frivolous; it’s the patient’s, and my job is to listen 🙂
2) Never, ever underestimate the power of a puppy.

I had a patient who rated their pain at 10/10 even before we engaged in any activities. I couldn’t begin to imagine the pain they were in, but I did my best to listen and determine what I could possibly do to help the patient achieve his goals despite the pain.
As we began some bedside exercises, his roommate’s family brought in a beautiful, serene, small dog. I noticed a glimmer in my patient’s eyes and beckoned the family member to come over for a little visit. The patient was able to gingerly lift his hand up to stroke the puppy’s soft ears, then he closed his eyes for a moment and said, “Wow. For just a moment there, my pain was down to a 6.”
It was a beautiful and humbling moment. I may have an idea about what would be most effective for a patient, but it’s important to be flexible in the moment and remain open to the idea that something more effective might have just walked in the door.
3) Sometimes, a laugh is worth a thousand interventions.
In school, our professors taught the importance of the “therapeutic use of self.” Simply put, the rapport we develop with our patients can facilitate healing, along with our official interventions. Personally, I have struggled to determine how my “full of energy and laughter” personality can be best channeled into a professional demeanor that is authentically positive yet perceived as appropriate in a medical setting. One of my internship goals is to fine tune my professional persona so that it best serves my client’s needs.

In the last 2 weeks, I have been incredibly pleased to find that the SNF environment is often full of laughter!
One morning I observed in awe as my clinical advisor turned a patient’s tears into laughter within a mere minutes of walking into the room. The patient was upset that she wasn’t getting better quicker, and the therapist was able to make a joke that revealed to the patient that perhaps her expectations had been unrealistic, and that she was doing very well all things considered. Many physical and occupational therapists have counseled me that an extra 5-10 minutes of rapport building at the beginning of a session is often a wise investment for the remaining 30-80 minutes.
As Victor Frankl said about the role of humor in “Man’s Search for Meaning” (which details his experiences as a concentration camp victim in WWII), “Humor was another of the soul’s weapons in the fight for self-preservation. It is well known that humor, more than anything else in the human make-up, can afford an aloofness and an ability to rise above any situation, even if only for a few seconds.” These moments of transcendence are so important during the rehabilitation process; they may not always involve laughter, but I certainly have come to terms with the role humor can play in the healing process over the last 2 weeks!
4) The meaning of suffering…or the suffering of meaning.
Lest my puppy and laughter-filled stories give an unbalanced impression of the SNF environment, I must point out a basic reality: every single one of the patients I’ve seen is suffering, or has suffered, in some profound way. As Frankl argued in Man’s Search for Meaning, suffering is like a gas; it fills whatever chamber it enters completely, no matter how big or small the chamber.
Yet as Frankl also argued, “I would say that our patients never really despair because of any suffering in itself! Instead, their despair stems in each instance from a doubt as to whether suffering is meaningful. Man is ready and willing to shoulder any suffering as soon as long as he can see a meaning in it.”
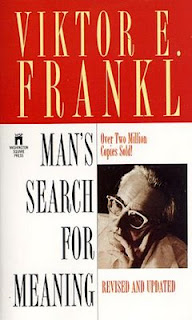
I would say that most patients need to see a meaning or purpose to their recovery, if not their suffering itself. The meaning could be as simple as, “I need to get better to take care of my husband” or “to see my grandkids again.” It could be more complicated, as in, “I need to get better so I can prove that I can live safely on my own, without anyone’s help.”
Many of the patients who struggle the most with the rehabilitation process don’t see any purpose or meaning in it. They may not understand the purpose of the specific exercises (“Why do I have to do this silly obstacle course around the therapy gym?”), or they may not see the big picture purpose of their recovery (“Why should I try to get better if I’m just going to get sick again?”).
I’ve noticed that occupational and physical therapists are, on the whole, somewhat biased towards recovery; of course, recovery is the purpose of our professions. However, I believe it’s important for us to consider the depth to which some patients don’t understand the meaning or purpose of recovery. Nearing the end of life, some patients do not wish to improve on their conditions and prefer to be “left alone,” as one patient vehemently told me one afternoon. In this case, our job is not just to provide an environment where they will “get better,” but to help the patient understand why getting better will help them.
You may think this is self evident; better is better, shouldn’t that be enough? The problem is, getting better involves pain, exertion, embarrassment, and many other uncomfortable emotions for many patients. In the short term, it is almost always more comfortable for a patient to just stay in bed. As Nietzche said, “He who has a why to live for can bear almost any how.”
I knew going into this profession that occupational therapy involves deeply personal, psychological and physiological issues; what I did not fully recognize until now was how deeply philosophical it also is. I hope that in the coming weeks I can impress upon a patient not only the “how” and the “what” of their rehabilitation process, but also the “why.”
_________________________________
*The fieldwork experiences are designed to help advance the student from academic to clinical competency. Each student is paired with a clinical instructor who’s a full time occupational therapist with at least 3 years of experience. After shadowing that instructor and learning the ropes, the student takes on a progressively larger portion of their instructor’s caseload, with their close supervision and guidance. They become a member of the treatment team for 12 weeks and are given constant feedback and guidance. It’s a wonderful model for learning!
No Comments
Carolyn Bousfield
Hi, Cheryl,
You have a wonderful enthusiasm for life, and I can tell you will make a huge difference in your patients’ lives. I am an Occupational Therapist, and I have recently been diagnosed with Rheumatoid Arthritis. Mine has hit my hands more than my feet; it sounds like yours has affected your feet more. Is that true? ( I found the link to your blog in an Arthritis magazine; thank you so much for posting out there 🙂
Are you delving into the gluten-free baking to address your RA issues? I am considering eliminating wheat for that reason.
I would love to know more about your situation and where you are now in relation to your OT degree.
Carolyn
Cheryl Crow
Hi Carolyn, i’ts great to “meet” you virtually! I’m sorry to hear of your recent diagnosis of RA. To answer your question about my inflammation patterns, I have had more chronic pain on my hands than my feet (my right first finger MCP and thumb CMC joints specifically), but my metatarsal inflammation on my right foot has been more acute and debilitating when it’s occurred. So, I deal with mild stiffness in my hands pretty much all the time, with periods of moderate to worse pain in my right MCP and CMCs, but when I have the foot pain (a few times a year depending on the year), it’s so bad that I can barely walk. If you are seeing one pattern already, it’s that RA is not always predictable!
To answer your other questions: Yes, I tried a gluten-free diet 3 years ago and stuck with it because it helped with some GI issues. I did not see a huge improvement in RA symptoms but it’s possible there has been one (perhaps my body would have been more inflamed had I not gone gluten-free). My best advice for that is to learn to love foods that are naturally wheat free; I absolutely love most Japanese, Thai, and Vietnamese dishes and many are naturally gluten free (watch out for soy sauce, thought!). Regarding where I am with OT, I finished my Masters in December and am currently studying for my board exam in April. I’m also narrowing down where I want to work afterwards. Joint protection is a pretty big factor for me; for example, I sincerely enjoyed my Spinal Cord Injury Rehab position with adults in California, but I’m fairly certain that the job requires too much strain on my hands for it to be ideal long term (although I could possibly work with the pediatric SCI population). Right now I’m very interested in pediatrics (school setting or outpatient) and geriatrics (skilled nursing setting most likely). Where do you work, and how has your RA diagnosis affected you? Great to connect with you! – Cheryl
Sydney McCready
Don’t spend too much time struggling to fit your demeanor into a “professional” one, you will find that one of your gifts is to redefine for others a more joyous definition of “professional” by watching your love wash happiness over the patients that you work with. You won’t be the typical OT, but therein lies the blessing! You will be your kind of OT and that is the best kind! Others will be better at what they do as a result of observing your habit of turning things on their head to view the problem from another angle. That’s where the fun is, that’s where the mystery lives that you will solve each time you engage your listening heart and mind to a spoken or unspoken need for special tissue boxes. Have fun, let your gifts flow!
Xoxo
Sydzo
Peggy Crow
Cheryl, we loved reading this! You framed your thoughts beautifully and we learned a lot. Your insights into the philosophical aspects of OT are fascinating. You will be such an asset to your profession. You always amaze us, XO Mom & Dad
Cynthia
I’m totally amazed at what you are, do and think, Cheryl. Each time we talk or listen to you, it’s a new experience. It’s wonderful that you are such a kind, good person — genuinely. Love Cynthia MOM
Regan
Thank you thank you thank you, Cheryl! This is beautiful, insightful, and touching.