10 Years with Rheumatoid Arthritis: What’s the Impact?

I recently realized that I have lived with rheumatoid arthritis (RA) for ten years, or roughly a third of my life! In that time I’ve graduated college, traveled to 12 different countries, lived in 3 states, traveled to/through over 15 states, started swing dancing, adopted 2 kittens, earned a Masters degree in occupational therapy, got married, bought a house, and more. I’ve also spent a considerable amount of time and money managing this chronic illness and mitigating it’s effects so I can live with the best quality of life possible.
In honor of my diagnosis anniversary, I’d like to share how RA has (and hasn’t) affected my life over the last 10 years.
Understandably, most people assume that joint inflammation and/or pain has the biggest impact on the life of someone with RA. However, if I really look at how my life has changed due to my diagnosis, the impact extends far beyond the physical. Using the Occupational Therapy Practice Framework as a general guide, I’ve created a handy pie chart which shows the seven areas of my life that have been most affected by RA. I will explore each in detail below, starting with the top right. 
1) Physical Effects of RA:

For those who don’t know, RA is an autoimmune disease. In RA, your immune system mistakenly attacks the lining of your joints, which has a cascade of effects beyond joint inflammation (“arthritis”), pain and degradation. Although arthritis is in the name because joint inflammation is a main effect, RA is in fact more similar to lupus than osteoarthritis, which is caused by joint cartilage breakdown over time. RA has “systemic” effects on other organs, such as the heart, lungs, and vascular system (explored in detail at the link above and here).
So, what has that meant in my life? Well, my levels pain, inflammation and fatigue have varied vastly over the last 10 years. I’ve had years at a time with absolutely no symptoms (“medicated remission”), but I’ve also had a couple of “flare-ups,” where pain and inflammation have increased to the point that I have to change my medication regimen and how I approach tasks.
On the average day, I feel a dull ache in my “distal” joints (farthest away from the core – think fingers and toes, not shoulders and hips) which is slightly worse in the morning and at night. I intermittently have cricoarytenoid arthritis, or inflammation of a small joint in the throat, which results in dyspnea. Dyspnea means difficulty breathing or an “unpleasant awareness of the work of breathing.” Overall, I have been very fortunate to respond well to my medication regimen, which has kept my inflammation at bay.

Despite my mild level of daily joint inflammation, I experience many systemic effects of RA, including chronic eye inflammation, gum inflammation (leading to hefty dental bills), non-iron responsive anemia, occasional fatigue, and some gastrointestinal symptoms that may or may not be related to RA depending on whom you ask. The gastrointestinal issues have led me to adopt a nightshade and gluten free diet.
I also experience medication side effects, including increased risk of infection (which means I must be very careful to wash my hands and practice other “infection control” measures), digestive issues, and fatigue.
In summary: While I’m very lucky to respond well to medication, my life has been affected by the direct and systemic effects of this disease and medication side effects. The hardest aspect for me is not managing my physical symptoms but rather the unknown. If I’m currently in mild pain, next week will I have a huge flare-up, or will I be in medicated remission for the next 10 years? No one can answer that, which makes life planning difficult. Then again, we all ultimately don’t possess answers regarding our physical future…but more on that later.
2) Daily Routine: The Why, and the How.
My physicians prefer my RA be controlled 100% through medication, which would allow me to live a completely “normal” life without making any modifications. However, as an occupational therapist I prefer to tweak my daily activities so as to minimize stress on my joints.
The way I see it, my joint inflammation at any given moment is partly a result of my immune system attacking my joints, and partly a result of the additional stress I put on them as I engage in daily activities. Medication addresses the former cause of inflammation, but not the latter. I can control the way I approach daily activities, so I owe it to myself and my long term joint health to do so! Joint protection has become a part of my daily routine at almost a subconscious level. Here are just a few of the ways I approach activities differently to prevent further joint damage:

Dressing: I take my RA into account when selecting clothing. Typically I avoid shirts with lots of tiny buttons, as they involve lots of repetitive motions of the small hand joints. I also am extremely selective with my footwear, with the dual goals of minimizing stress on my foot joints and making the shoes easy to put on and take off (see my previous post on RA-friendly shoes, where you will discover my obsession with Danskos!).
Cooking: A few simple kitchen modifications I’ve employed include: using an electric can opener rather than manual, using a smaller Brita water pitcher rather than a larger/heavier one, purchasing very good/sharp knives to miminize the amount of force I must use to cut things, using an electronic food processor and kitchen aid rather than manually stirring food, using “mass movements” (shoulder/elbow/trunk) to open items rather than relying on the small hand/wrist joints whenever possible, and asking for help with lifting large/heavy items. When I am lifting any object in the kitchen, I follow the basic rules of joint protection.
Computer/phone use: I take frequent stretch breaks at the computer and always use a mouse rather than a trackpad. Mousing puts less stress on my MCP joints (knuckles) than using the trackpad (and the MCP joints tend to be most affected long term by RA). I’ve also started using talk-to-text programs when I’m not in public, such as Siri. I find it’s much easier to dictate a short message this way, plus it’s way faster than trying to finagle with the small keyboard on the iPhone!
(I’m time travelling back from the year 2019 to say that if you’d like to learn more about how daily activities are affected by RA, and to learn about life hacks I’ve developed since this post was written, check out Arthritis Life!).
3) Financial and Health Management Adventures with RA
Health management and financial costs affect everyone with chronic illness, regardless of whether one is experiencing symptoms at the moment. I’m sharing these costs (financial and time burdens) not to complain, but just to paint a realistic picture of what managing this disease entails. RA appears to cost me 26.8 to 74 hours of time per year, and $2800-$8000 per year depending on my insurance. Note: the financial costs are just what I directly pay; my insurance company is paying over $20,000 a year for Enbrel or Remicaide alone.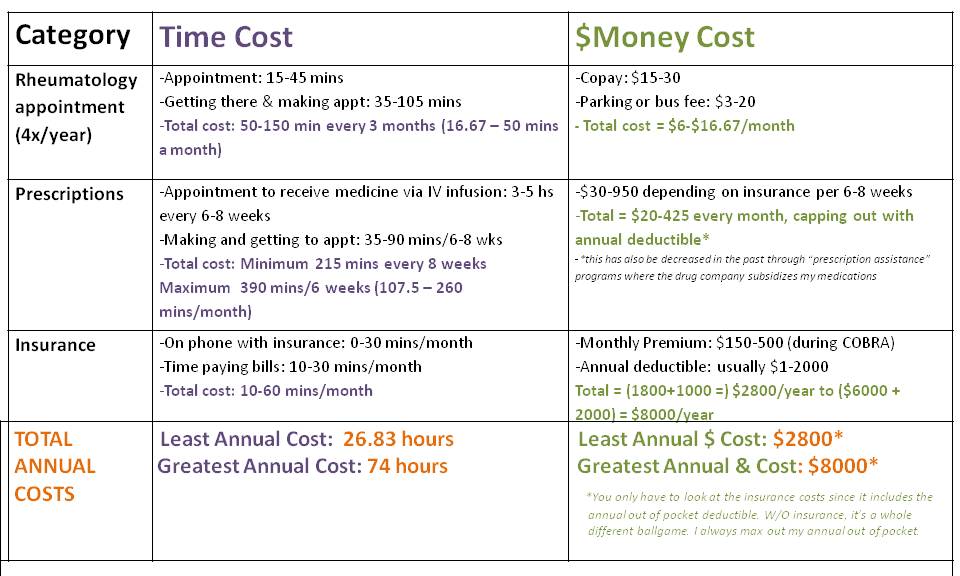
4) Social & Emotional Effects of RA:

As marriage became more of a real prospect in my mid to late 20s, I found that anyone entering into a romantic relationship with me would consider the potential lifelong effects of the disease. My impression is that the disease itself was seen as a negative, but the way I managed it was seen as a positive. I also think I self-selected partners who shared my view, which is that you never know what physical or mental condition someone might develop when you make that lifelong commitment. We all know that we could be hit by a car tomorrow and our whole lives could change, so putting extra stock in the physical when making romantic relationship decisions is unwise.
That being said, when you enter into marriage after having experienced health issues, the phrase, “In sickness and in health” certainly carries more weight. In fact, the only time I became tearful during my wedding ceremony was when saying those words!
Regarding family and friend relationships, I’ve had wonderful support from both groups. The only small point of friction has been when I have felt peer pressured to stay up late, over-exert myself and not give my body the rest it needs. My peer group largely has subscribed to the “I’ll sleep when I’m dead” approach, which simply doesn’t work for me (or most people with an autoimmune disease). My body starts shutting down when I get less than 8 hours consistently a night. I’ve learned to be assertive with this, and deal with “FOMO,” or “Fear Of Missing Out.”

On the positive side, RA has paved the way for me to make some additional friendships and relationships. I’ve met other patients through the Arthritis Foundation, at the summer camp in the northwest as well as other volunteer and advocacy adventures. I’ve also met some amazing folks through social media and blogs, such as RA Chicks, RA Warrior, Creaky Joints, and RA Guy. Lastly, I’ve recently made connections through Tumblr with some inspirational people through Arthritis Humor.
Emotionally, the hardest times have been when I’ve had unexplained symptoms. This happened the full 2 years before I got diagnosed and has reoccurred a few times since then. As someone who prides herself at the ability to get to the heart of the matter, I’ve found it frustrating when I can’t figure out what is causing a particular symptom and how/when it will go away.
I also have felt anxiety about the future, due to not knowing how RA will affect important life roles that I hope to have such as being a mother someday. Will I, like some women with RA, go into complete remission during pregnancy but then have a huge flare-up after giving birth and barely be able to hold my own baby? Or will I go into lifelong remission after having a child, like my great aunt did?
The unknown for me is probably the very hardest aspect of this disease. If I knew that I’d have X effect for life, I could habituate my mind and approach to it, but unlike a situation such as a complete spinal cord injury where the prognosis is pretty clear cut, autoimmune diseases have varying courses for each individual. The upside is that I have the potential to feel great in the future, but the downside is that I will always have to handle the unknown and lack of clarity on what is happening in my body.
5) School & Career w/RA:

During the first 6 years of my diagnosis I explored some truly amazing careers, including: working in a private school for children with severe developmental disabilities, program development at an international photography and youth storytelling nonprofit, and organizational development and training at a top 10 academic medical center in Seattle.
During that time, I did a ton of soul searching about what career would be the best fit for me long term, and RA did play a role in my decision making. I decided I wanted a career where my primary purpose was directly helping people (individually or in small groups). The career had to be flexible enough that I could work in a variety of settings, regardless of my potential joint inflammation.

Occupational therapy emerged as the perfect fit due to the large scope of practice and variety of practice settings. It also has a lot of part time work availability, which appealed to me as I’m hoping to work part time when I have kids. Additionally, OT is an intrinsically optimistic profession. We will rehabilitate or compensate for any physical or mental condition so that our clients can “life life to it’s fullest.” OTs want to maximize the amount of function one can achieve despite any illness or injury, and that philosophy appealed to me as it’s very inclusive of a diagnosis such as RA.
As an OT student, I experienced occasional pain from handwriting. However, my vast experience with the health system and my own journey as a patient generally have a positive effect on my school and career.
One positive effect of my diagnosis on my career is that I can empathize with my clients’ interest in knowing “the answers,” and their frustration when they eventually discover that no one knows them. People can tell you what is most likely to happen, but no one in the health or education system is a fortune-teller. I really identify with my clients’ (or family’s) frustrations over how difficult it is to make decisions off of what sometimes feels like incomplete information. Once you understand how complex the human body is, it seems self-evident that no one can give you the answers, but I vividly remember my experience of the healthcare system before I became a provider, and the profound disappointment I felt when I was confronted with this reality. I try to really acknowledge this aspect of my clients’ experiences and validate their concerns.
6) Hobbies & Travel with RA:
My choice of hobbies has certainly been affected by my diagnosis. I used to run almost every day, starting in high school through to a couple years after my diagnosis, but eventually decided to try forms of exercise that would be less strenuous on my joints: swing dancing!
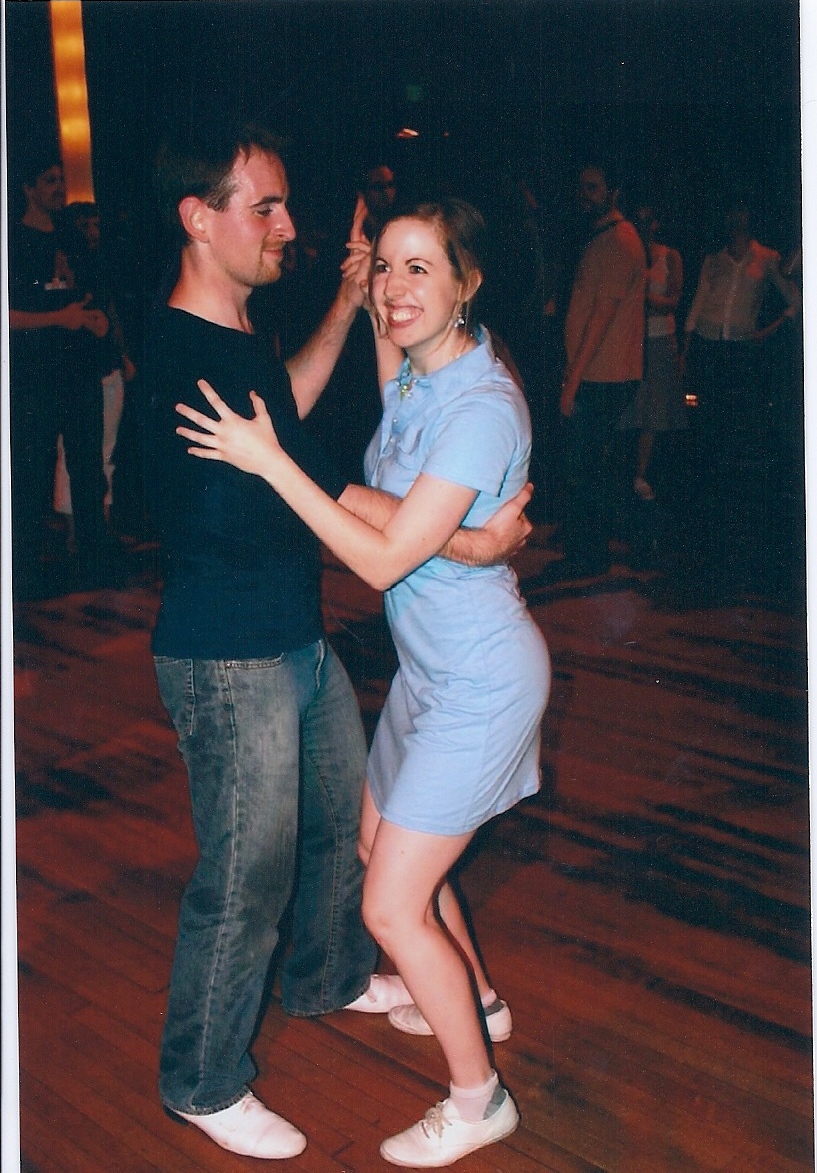
In my video “Why I Dance,” I shared how dancing grew into a huge part of my social life. I have to be careful about certain moves which cause strain on my small hand joints, but overall I’m fortunate to be able to take part in this wonderful community despite RA.
Swing dancing is a great example of how RA took something away from me, but I discovered something equally meaningful in its place. Do I miss running and soccer? Absolutely, especially on clear, beautiful Seattle days. On a purely physical basis, I prefer the endorphin release of soccer or running to swing. However, when I look at the whole package of the activity (with the social and musical elements), the trade-off is without a doubt worth it.
Now, onto travel. Yes, I have been to 14 countries since my diagnosis: Belize, Fiji, New Zealand, Japan, China, India, Turkey, Czech Republic, Germany, Belgium, Netherlands, Ireland, England, and Canada. Phew!

The biggest effects of RA on my travelling are the prescription and health management aspects. My first international trip post-diagnosis was to Belize, where I volunteered for a great organization called Cornerstone Foundation. I was only planning on staying for 3 weeks but I ended up staying 3 months, which meant that I needed additional medicine. I was on Enbrel at the time, a twice-weekly self-injection medicine which MUST stay refrigerated. My mom graciously helped me research how to ship it, but found out that it is illegal to ship things on dry ice to Belize due to drug concerns. So, guess what our solution was? My mom took advantage of low ticket prices and decided to bring the medication to me – now, that’s what I call customer service!
The drama wasn’t over at that point, however – during my last 2 weeks in Belize, there was a strike by the electrical supplier to the entire region, so we had no electricity to run the refrigerator! Luckily I was able to keep my medication cold, but it just goes to show some of the difficulty of travelling with RA.

During my other travels, I sometimes had to simply skip a week or two of medication. I was lucky not to experience any adverse affects with this approach. I also had to get “vacation authorization” to pre-fill extra amounts of my medications for longer trips.
Since I switched to Remicaide, the infusion-based medication which is administered every 6-8 weeks, the biggest travel concern has been coordinating my travel dates so that they do not conflict with my medication schedule. For example, I had to get an infusion the week before my wedding so that I would be covered through the honeymoon. This has also affected my current travels to China, as my husband is there on an extended business trip. Luckily, my infusion schedule overlapped with a few weddings I wanted to return home for anyway!
Spending extended time abroad would be anxiety-provoking to me from a medical standpoint, because I have found that errors or confusion are more likely each time you introduce a new provider to the mix. However, short trips for me have been manageable with some work upfront.
7) Philosophical Effects of RA: The Biggie.
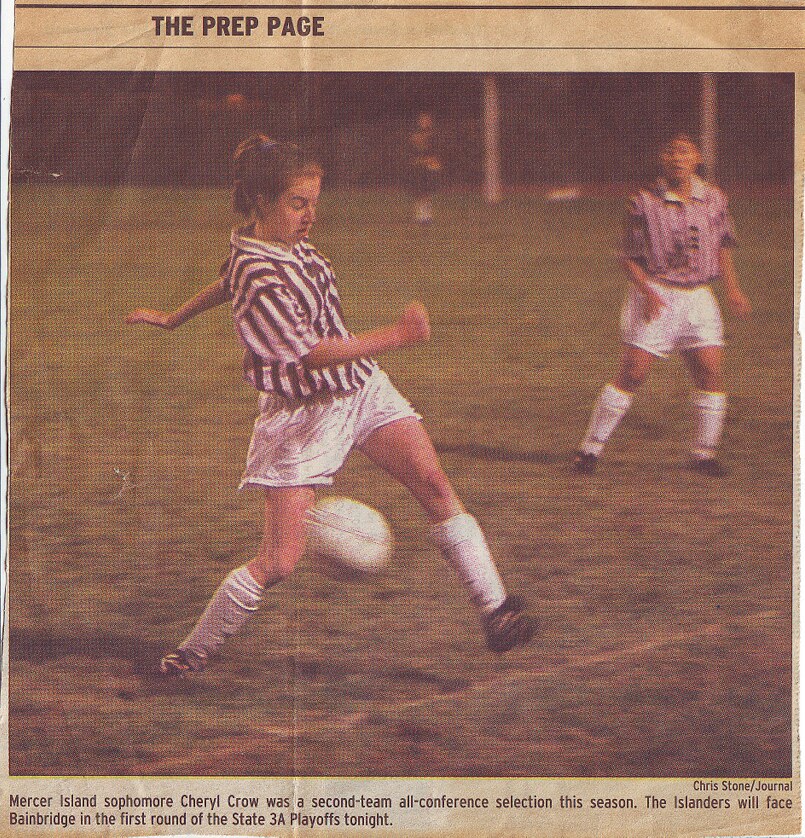
For years, I believed that if I treated my body as a temple, I would reap the rewards of my efforts. I ate well, avoided recreational drugs, exercised vigorously daily, and as a result had a body that operated smoothly and efficiently. I ran a 5:30 mile, weight lifted 5x/week, and never subbed out of my high school or college soccer games (clocking in 90 mins/game).
Experiencing my body break down in the absence of anything I was willfully doing felt like a double betrayal. It was a betrayal of myself BY myself (there wasn’t even an outside virus to blame!), and it was a betrayal of a philosophical system I didn’t know I had, which is that I can protect my body from harm by doing “the right things.”
I know now that my years of good health were partly a result of my actions, but also a result of good luck. My baseline state of good health enabled me to maximize my fitness and do great things, but I wasn’t in control of that original baseline state. In my gut, I suppose I knew that I was lucky to be in good health; I had seen other athletes fall victim to injuries and seen friends/family fall ill to various diseases through no fault of their own. There is a transition period, however, between knowing your body is not invincible and accepting it.

So, what or who is to blame when the body betrays the body? In my own belief system, there was is no god or greater power or force to blame or help make sense of it. There isn’t a “reason” or meaning to my diagnosis; it just is. All humans are mortal, and all human bodies are subject to disease and illness. There are certainly preventative measures we can take to minimize risk, but there are no surefire ways to prevent yourself from all possible illnesses and injuries.
My diagnosis led me to confront the infallibility of my own body, which in turn made me confront my own mortality. The realization that “my physical body is not completely under my control” naturally led to “my physical body will eventually not work anymore.” Accepting my mortality has been crucial for giving me a strengthened sense of purpose and urgent desire to make a meaningful life. The graph below outlines the interplay of these factors.

The fact that I am going to die someday gives immediate perspective to any situation. My “bible” of sorts is a combination of “Man’s Search for Meaning” and “Tuesdays with Morrie.” Both of these books deal with the concept of death straight on. While Morrie is religious, the basic truths he utters are equally applicable to agnostics and atheists.
“Aging is not just decay, you know. It’s growth. It’s more than the negative that you’re going to die, it’s the positive that you understand you’re going to die, and that you live a better life because of it.” -Morrie Schwartz, in Mitch Albom’s “Tuesdays with Morrie.”

Confronting my mortality and the mortality of all humans has been the compass around which I live my life and make decisions. It’s the only thing I know for sure. I am alive now, I will die someday, and I desperately want to leave something positive for the world behind, to make my life worthwhile. There is no inherent meaning to my life, the only meaning comes from the good (or bad) actions I choose to take during my limited time on earth.
Sure, I knew I was going to die on some abstract level before I got diagnosed with RA. But there is something about a stark, black and white diagnosis that makes the abstract concept of mortality more real. This is perhaps the greatest gift that has arisen out of my diagnosis.
Conclusion
In conclusion: the effects of RA have extended far, far beyond the physical in my life. My diagnosis affects everything from micro-elements of my life (such as how I approach simple daily living tasks in the kitchen) to macro-elements (such as my sense of purpose and acceptance of my mortality).
I hope that this exploration has helped the reader see RA as much more than simply autoimmune-caused “joint inflammation!” I’d love to see charts of other peoples’ top life effects of RA – feel free to share your experiences in the comments section.
33 Comments
Simran Sharma
Thank you for sharing an amazing information.
Pingback:
Pingback:
Richard Hoover
Thank you for sharing your experience! Your approach is very inspiring!
Michael Treloar
Thanks for the information. sounds so great and helpful. Kudos!
Kerry
Thanks for sharing your story. Just diagnosed last week. I started my first dose of methotrexate and so far , so good. Tired but strangely enough , I feel at ease when I’m tired. The anxiety goes away. Your approach to RA is inspiring. Best wishes to you.
Minion
Hey sorry to hear abt u. Long journey ahead fr all of us. Stay strong n all the best!
Minion
Loved reading ur post. I just completed 10.5 yrs..i m 28 now, n only i know what i went through everyday. Wish u the best in life.
Cheryl Crow
Thank you so much for taking the time to respond, best of luck to you!
Smits
Hi Cheryl…. i have just been diagnosed with rheumatoid arthritis and it is nearly impossible for me to accept it. I have seen my mother go through so much of pain in last 20 years because of this. I don’t know what to do to make acceptance easier. I am not able to think about any positive thoughts of how I will go through the problem. I don’t know how I will live such a painful life. Please help.
Cheryl Crow
Hello,
Thank you for getting in touch. I’m sorry you were diagnosed and that your mother suffered so much. The current thinking is that people who receive early and aggressive treatment with the current, best medications will have MUCH better long term outcomes than people in prior generations (such as your mother) who didn’t have access to the current treatments. So, I think there is a scientific basis for more hope in your case. However, I think that grieving and being upset is a normal part of the process of coming to terms with your diagnosis, and it might be beneficial to just sit with those feelings for now and not force yourself into acceptance before you’re ready. Are you happy with your medical team? Having a provider whom you can trust and who is supportive can make a huge difference. Also, you might want to find an “Arthritis Introspective” group near you, to connect with other people who are going through what you’re going through: https://www.arthritisintrospective.org/ I wish you the best and please let me know if you have any more questions. My journey has gotten more complicated since having a child, so I will be providing a follow up post to this one sometime in the next year or so.
Farah
Hi Cheryl, I stumbled upon your blog recently as I was searching for stories on people who have lead a successful life with RA. I was diagnosed 4 years ago at the age of 25. I am currently in remission and hardly ever feel the effects of my RA other than fatigue. This post helped me to understand that the things that i have found difficult (fatigue, social life) is something others struggle with. And that I also maybe holding myself back from things I am actually capable of doing such as traveling but have told my self it would be too hard now. The reason I was searching for this topic is because my boyfriend and I have been discussing marriage and having a family in the near future, and I am not sure if I am capable keeping up with this life that I want to give him so badly. It inspires me and comforts me to know you have been able to do this successfully. My question for you is how you are feeling about managing a child husband and career? I am in a similar field as you (speech pathology) and this is one of my biggest fears as I love my job. Also if the process of carrying a child was difficult without taking medication? Thanks so much for sharing your experiences, I really appreciate it.
Cheryl Crow
Wow, thank you so much for your thoughtful response, and I’m so glad to hear you are in remission! My personal response about your decisions about marriage/raising a family is that if it’s something that’s important to you, you *will* make it work! It might not look the way you imagined it, but having kids *rarely* looks in real life like we imagined it would before we experience it. In other words, I wouldn’t wait to make the decision until you have a completely clear picture of how it will work out, because even if you created a clear picture, the reality of the future will likely be full of unexpected twists and turns. Perhaps it’s most useful to go with your gut in this case and trust that you can make things work. Just my 2 cents!
For me, managing my career has been one of the least difficult aspects of becoming a parent, which has been pleasantly surprising. I feel the same energy for my field of OT as I did before, but I am working part time to allow extra time with my kiddo, as well as time for appointments. I had a really great pregnancy (went into unmedicated remission) but extremely difficult post partum period, which apparently is the norm for many people with autoimmune diseases. I would say just make sure to have a ton of family/friend/whatever support you can get, in case things get rough. Having a baby is really hard for everyone, regardless of having a diagnosed disability, so I would not let that stop you at all – it may be hard for you in different ways than the “average” mom, but you can make it work – I actually posted about post partum strategies for moms, feel free to check it out! For me personally, the emotional and psychological aspects were more challenging than the physical, when it came to adjusting to being a mom, and I’ve learned to be more patient with myself and “go with the flow” more, which can be hard. It truly is so different for each new parent, and from what I’ve heard the experience is different with each child one has, so it’s very hard to predict how you will feel beforehand. Good luck and please keep me posted on your plans! -Cheryl
JML
Thanks for this post. I’m coming up on my 10 year “anniversary” and it was nice to read about someone else’s journey. My outlook is much like yours.
Christine Ross
Hi Cheryl, Thanks so much for writing this blog of your experiences living with RA. I was diagnosed with RA 14 years ago and although I receive great support from family, friends and my medical team, there have been times when I have felt quite isolated and alone. I can relate so much to many of the issues you talk about – the difficulty of travelling with medication, dealing with chronic pain, fatigue! I remember a time when we were travelling in Italy and needed to find a fridge for my medication – even though we did not speak Italian, we were able with hand gestures and the odd word, to get our message across. People went out of their way to help, relieving what could have been a very stressful situation.
I love your positive attitude and your determination to live a good life in spite of living with this disease. Recently, I spent 3 months in hospital. I had developed lung complications – a side effect of my medications. I received amazing care and after many tests, lung surgery and many ups and downs, am now almost fully recovered.
I see from your honeymoon photos that you have visited New Zealand. I am a ‘Kiwi’, although living in Perth, Australia for the next few years. The background of your photo looks familiar – perhaps somewhere in the Milford Sound? I hope you enjoyed your stay.
Thanks again for sharing your experiences! Keep well!
Kind Regards,
Christine
Pati Biancalana
Reading your article has been inspiring! I’m 57 years old and have just been diagnosed with RA. I see that you live in Seattle..? My husband and I would love to retire there, but I’ve heard so much about the humidity causing lots of problems with joint stiffness and pain. Do you find your location more challenging during the rainy season? Thanks so much, again! Be well! Pati
Cheryl Crow
Hi Pati! My best advice regarding the weather and RA is to just try different places and see how it affects you specifically, because it seems everyone is different. I personally feel more stiffness in the heat, regardless of humidity, which I know is totally opposite of many people who feel more stiffness in the cold or humid climates. It’s just one more way in which these diseases affect everyone differently! Good luck on your journey!
Reed
Pati…. riding the long road plaster cast 🙂
Ally
Hi Cheryl,
This isn’t the most recent of your posts, but I just checked out your blog for the first time! I am learning to deal with a chronic pain diagnosis myself and appreciate your words. The past 15 years of pain is one thing… now I am learning to accept that it is something to manage, not cure, and I am trying to unravel the deeply ingrained message that if I [tried harder/did more/sucked it up/was better at life], I wouldn’t have these problems. Of all the emotional relationships pain impacts, it’s hit hardest my relationship with myself.
From a dancer’s perspective, it’s inspiring to know that you can live with RA + get 8 hours of sleep a night + still keep up with dancing. I haven’t been fitting it all in lately but it clearly can be done! 🙂 Something to work toward.
I was wondering if you’ve had any experience with the TQI diet — http://toquietinflammation.com/ — it was recently recommended to me. Probably a lot of things you already know, but if you’re not familiar with it, there’s some interesting stuff in the books!
Best of luck with your impending birth!
Cheryl Crow
Thanks for taking the time to read and respond, Ally! It is so true about the shift in mental approach that takes place when you have a chronic rather than acute condition. I’m sorry to hear that this is a burden you must bear, butt sounds like you are on the right track and I wish you all the best as you continue to learn new ways to manage your pain!
Sleep has been so crucial for me, physically and mentally, and it’s my #1 concern for my transition to parenting an infant/baby/toddler/child! It’s always hard to find a balance but I hope we both can find one!
I have not tried that specific inflammation management diet. I currently am gluten free and nightshade-free, both of which were recommended on the basis of decreasing inflammation. I have always been curious about whether my symptoms would improve if I did a more “hard core” diet, but at some point it becomes a cost-benefit analysis about quality of life, and since my pain and inflammation have been managed pretty well with my current diet and my medication regimen, I am not trying any additional diets at this time. Let me know how it works for you, though! Hugs!
Gery'sBeautyBlog
Hi Cheryl,
I am honestly wow-ed by all of your accomplishments… Im 21 and was diagnosed with RA this year and I began in a wheel chair for almost four months. However I am not as accepting of this illness as others are, I find myself contantly upset and unmotivated and I believe its due to the huge loss of my social life and other activites.
I have so many dreams that I want to fulfill and I only hope to achieve your state of mind and perseverance!
And I truly resonate with what you wrote about “if I treated my body like a temple I would see the benefits of that in the future” and how that somewhat feels like a betrayal… however now I know I must do all that I can to live life to the fullest because I cant change the past.
Thank you for your post!
~ Gery.
Cheryl Crow
Hi Gery, thanks so much for getting in touch and for the nice words of support. I think that being upset and even unmotivated is a normal response to such a sudden life change that has taken away a lot of your former lifestyle. I think that many people go through the “stages of grief” when they get a diagnosis like RA, similar to the stages of grief when a loved one dies. In a way, it’s a part of your former life that is going away. It is definitely a process, and I think you will find that in time, you will adjust and find creative ways to participate in the things you really want to do, or you will find alternatives. However, do not feel guilty for going through what you are going through emotionally right now, as it is normal and an important part of the process! Remember that it has taken me 10 years to get to where I am, and it’s still an evolving process with ups and downs. I do find that I am happier when I focus on how I can still live my life to the fullest, because while RA has taken some things away, it has not even come close to taking everything away, so I find comfort in focusing on the many wonderful things I still can do and experience! I wish you the best and please keep me posted on how you are doing!
Gail
Your blogg is very inspiring to me. At the age of 62 I’m having the first symptoms of what I believe is Osteoarthritis, though my discomfort seems to move around from joint to joint. I’d had a background in Occupational Therapy as an assistant and have thought about re-licensing though I’m not sure I could find an area to work in with my joint issues. I’d tried working in hand therapy a few years ago and that was impossible. COTA’s work quite a bit in Skilled Nursing, and I’m leery of that specialization! A re-entry program would only allow me to work in Oregon. A special education position in a school might work for me, but jobs are few and far between. My symptoms were non-existent before this Oregon Fall and Winter began. For the last several years I’d been working as an ESL instructor in the Arabian desert and life was much easier in the desert for the joints. I hear about folks with joint pain who regain their youth, vitality and mobility when they get out of the high humidity and cold of the North West. A particular level of humidity is recommended! On the humidity monitor I have they recommend between 30% to 40% to 60% levels of humidity as being the best for joint health. I’d wondered if you’d had relief from symptoms in drier and warmer climates? If I’m living in the USA I’d like to re-locate to Arizona, but this kind of change wouldn’t be easy for me logistically or financially.
Cheryl Crow
Wow, you have had a lot of amazing life experiences, working in the Arabian desert sounds amazing! To answer your question, no, I have not noticed a relief from symptoms in drier and warm climates (and in contrast to most, I actually have slightly more inflammation in warm weather). That being said, I would always trust your body, and it sounds like you have a pretty clear pattern of feeling better in warm and dry climates. You might find that being a COTA in the schools, working with children with special needs, might be a great balance. Best of luck and please keep me posted on how you are doing!
Jane
Hi Cheryl,
I’m 47 and recently diagnosed but I know in retrospect I know it’s been lurking for years or a decade or more. Your explanation of your experience is so helpful. I have been a divorced mom of two sons who are 19 and 17 now. Most of my energy went into working and still does. I am self employed as a consultant in my field of 25 years. Can’t imagine becoming disabled but I’ve had a good taste of it for several months. I like my work – the income and validation from it. I love my sons and want to help them become adults. I love to run, ski, swim, play tennis, hike, and ride bikes and four wheelers. My dream is to have a house in the Rockies where I can do all that for the next 20 plus years. And to be an active grandmother to my sons future children. Those are my goals. Keep on keeping on!
Jane
Jane
Please ignore my typos. I’m posting via iPhone and I have fat thumbs.
Cheryl Crow
Hi Jane, I apologize for the delay in response! I’m glad that you got diagnosed and am sorry it was lurking for so long. Your activities and goals sound amazing, and I don’t see any reason why you won’t be able to achieve them! Keep me posted and best of luck to you!
Kari
Wow. This was a great read. I’m 3 years into my diagnosis. Diagnosed 2 months after my son was born – had extreme pain in my joints in hands, shoulders, and feet. Couldn’t even take care of my sweet baby. I have been through so many emotions with this disease but thankfully kept pushing through. Thankfully i still have my running and along with my son they keep my going. Reading this gives me even more encouragement – especially the travel aspect. I’ve been so scared to travel bc I would be away from my humira. Oh and i have the same pregnancy anxiety – the unknown is scary! Thanks for this!
Cheryl Crow
Thanks so much, Kari! I’m sorry to hear you were diagnosed after your son was born, that must have been SO hard because it’s already a difficult time with lack of sleep and adjusting to having an infant! I’m glad you can still run, that is wonderful. Yes, I’ve found that traveling hasn’t been as hard as expected – the unknown is always the hardest part. Thanks so much for your nice comment and i hope you continue to thrive!
Ruth Baldwin
Hi Cheryl, Thanks for such a thoughtful message. It seems like something I will read more than once because there are so many great insights. It is inspiring to see how you have thrived!
Cheryl Crow
I’m so glad that you found it insightful! I have been fortunate to have a really great care team (especially the 3 Rheumatologists I’ve had since I was diagnosed: one in New York, one in California and one in Seattle), which I think has helped set the stage for me to be able to thrive despite RA. Thanks for your kind message!
Jessica
Thank you so much Cheryl! I appreciate so much that you took the time to write this and share it. With RA, you see people living a normal life, but it’s hard to remember that they are dealing with the disease everyday. It has been almost 2 years since I was diagnosed and I think I am still in the “transition period” where I need to accept that I simply don’t have the same body that I used to. I find myself discouraged with being so fatigued after midday and feeling like I don’t accomplish much except the basics of keeping my kids going (preparing meals, cleaning up, baths, etc.) which is alot, but there are so many things left undone, which I think is common in a home with 4 kids, but I feel the weight of it even more so as I just don’t have the energy to do it.
RA has made me pay attention to the more important things and helped me focus on spending time where it matters most. It’s not hard to read a book to my kids or sit and visit with them, which they need me to do. Having RA makes it easier! Thanks again for sharing! You are a wonder!
Cheryl Crow
Hi Jessica! I can’t imagine how much work it takes to take care of FOUR children. Just the basics for one child are a lot for anyone to handle, even without RA! So I would say to be gentle with yourself and remember what a huge job parenting is! Energy and fatigue are such precious resources, as you mentioned. It can be difficult to know that you technically have time to get something done, but don’t have the energy at that moment. Usually it’s best to just listen to your body and give it the rest it needs, if you can…but it’s hard! Thanks for your thoughtful response and I look forward to staying in touch!